
Anxiety disorders are common mental health problems, with global prevalence ranging between 0.9% and 28.3%1. The disease burden of anxiety disorders is substantial as the disorders are associated with significant morbidity, disability, and healthcare utilisation. Although a wide range of pharmacological and non-pharmacological approaches are available in the treatment guideline of anxiety disorders, effective control of the disorders is still challenging2. Apart from pharmacological treatment, the advancement in digital technology in recent decades has presented new opportunities for assessing and treating various psychiatric disorders. Notably, anxiety disorders have been reported as one of the most promising interventional targets for technological therapies across all mental health conditions. Hence, the objectives of this article are to review specific clinical issues about anxiety disorders and to discuss the application of digital therapeutics in combating the disorders.
Anxiety disorders are a leading cause of disability worldwide, accounting for 28.7 million disability-adjusted life years (DALYs) in 2019, and are receiving more attention by virtue of the high incidence, the early age of onset, the tendency to relapse for a long time and the disabling nature3. In Hong Kong, a previous survey conducted in 2010-13 reported that the prevalence of generalised anxiety disorder, mixed anxiety and depressive disorder, and other anxiety disorders among Chinese persons aged 16−75 was 4.2%, 6.9%, and 1.5%, respectively4. Remarkably, the data on demand for psychiatric services at Hospital Authority (HA) reflected an increasing trend in the number of patients with mental illness receiving care in the public medical system4, which thus highlighted the significant local disease burden of mental diseases, including anxiety disorders.
People suffering from anxiety disorders usually experience excessive fear, nervousness, and avoid threats in the environment or perceived by themselves5. In addition, the disorders can also be accompanied by autonomic dysfunction and/or panic attack6. Apart from personal impact, anxiety disorders would adversely affect the patients’ families and society as well4.
While we are still in the battle against the COVID-19 pandemic, there are accumulating investigations reporting the impact of the pandemic on the mental health of the local population. For instance, Zhao et al (2021) reported that, after the peak of the second wave of the COVID-19 outbreak, 15.8% and 14.8% of the participants had anxiety and depressive symptoms, respectively7. Although not in a head-to-head comparison, the prevalence of anxiety reported in the study appeared to be higher than that in the survey before pandemic4. Besides, stress, anxiety, and depressive symptoms were more prevalent in those with shortages of preventive materials and negative perceptions of the outbreak. The results further suggested that reduction in income and unemployment were associated with more mental health symptoms7.
Besides, in a population-based study by Hou et al (2021), stress due to civil unrest and COVID-19 was demonstrated to be associated with a higher prevalence of probable anxiety and depression, whereas the effect of stressors on probable anxiety and depression is cumulative (Figure 1). Notably, the results further suggested that the probabilities of mental disorders were substantially higher among persons with fewer assets8. Hence, the findings presented the pandemic’s adverse impact and the potential role of socioeconomic factors on the development of mental illnesses, including anxiety disorders.
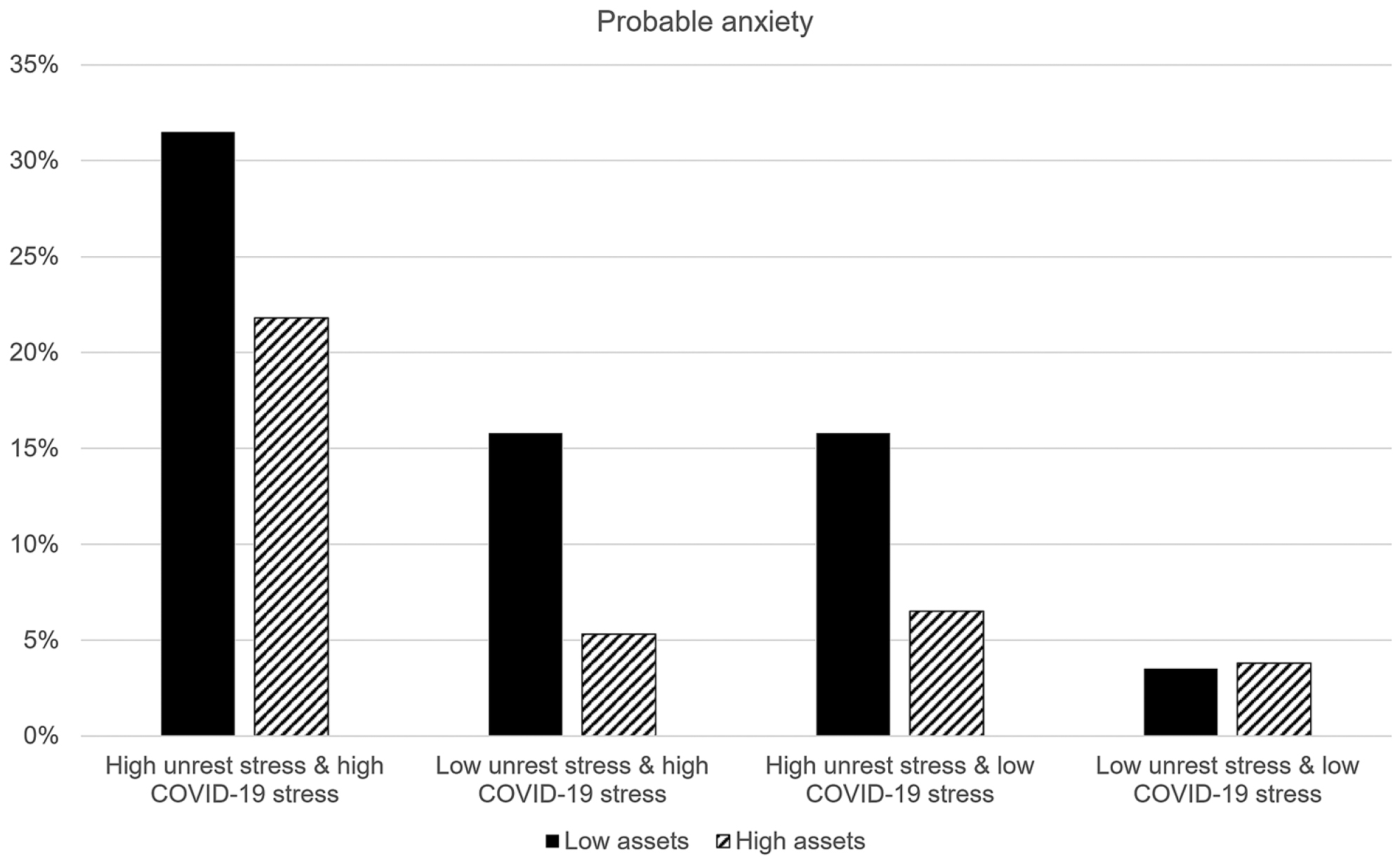
Figure 1. Prevalence of probable anxiety across different stressors among respondents with low and high assets8
Anxiety disorders are treatable with psychotherapy, medication, or both. Psychotherapy involves working with a therapist to reduce a patient’s anxiety symptoms. Cognitive behavioural therapy (CBT) is the most effective psychotherapy for anxiety disorders. It focuses on teaching the patients specific skills to improve their symptoms and gradually return to the activities avoided due to anxiety. CBT includes exposure therapy, in which the patient gradually encounters the object or situation that triggers anxiety symptoms to build confidence in managing the situation and anxiety symptoms9.
While CBT aims to build up the patient’s abilities to manage their problems, medications are usually for severe cases. For instance, the Food and Drug Administration (FDA) has approved several selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) for panic disorder, generalised anxiety disorder, and social anxiety disorder10. Previous clinical data advocated that most SSRIs and SNRIs were efficacious in controlling anxiety symptoms11. While adverse effects associated with SSRIs and SNRIs are usually manageable or short-lived, treatment-related sexual dysfunction, which may be durable and problematic, should be closely monitored10.
Of importance, clinical opinion suggested that the treatment plan for patients with anxiety disorders should be carefully decided based on factors including the patients’ preference, their history with previous treatment attempts, illness severity, comorbidities, availability of treatment methods, and costs12. Notably, it has been reported that patients with anxiety disorders are often hesitant to take psychotropic drugs due to the fear of adverse effects. Thus, patients must be well informed about possible adverse effects, interactions, safety warnings, and contraindications. If they are educated about the possibility that some early side effects might later decrease in intensity, compliance may be improved12.
Although many pharmacological and psychotherapeutic treatments are reported effective in countering anxiety symptoms, many patients are under-treated in reality. According to the Hong Kong Mental Morbidity Survey (2015), the 12-month mental health service utilisation was 35.9%, 16.0%, and 46.2%, respectively, for generalised anxiety disorder, mixed anxiety and depressive disorder, and other anxiety disorder13. Nonetheless, patients with psychiatric comorbidity had higher rates of service utilisation, whereas those with anxiety disorders alone were about three times less likely to seek help (Figure 2)2.
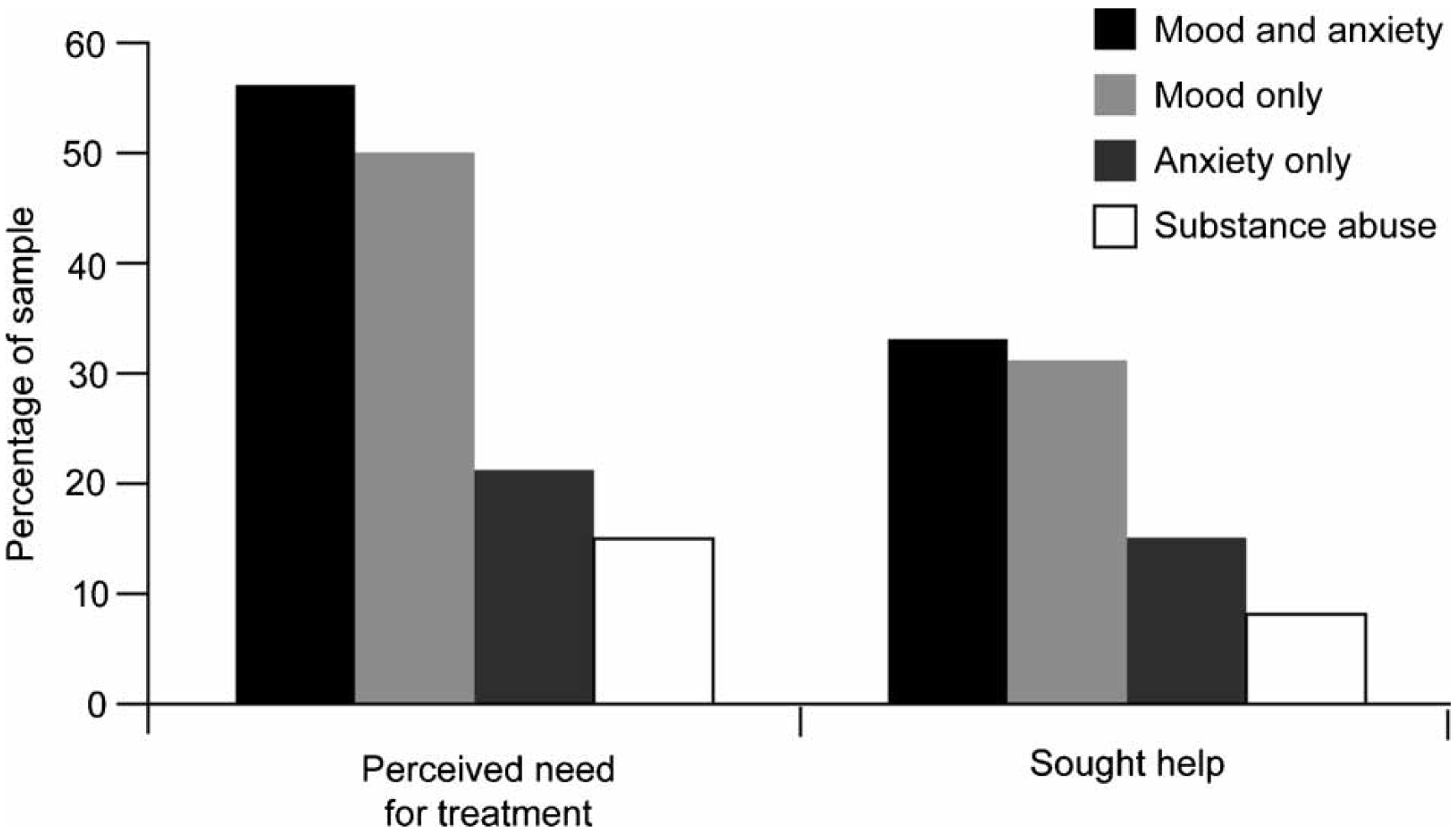
Figure 2. Help-seeking in patients with mood, anxiety or substance use disorder2
On the other hand, the difficulties in recognising and diagnosing anxiety disorders may contribute to under-treatment. Clinically, anxiety disorders are frequently complicated by the presentation of many different clinical features, especially major depressive disorder, leading to difficulties in recognition and diagnosis. Of note, comorbid conditions are particularly prevalent in the elderly2.
Pharmacological treatments are efficacious in a wide range of psychiatric disorders. However, the treatment-related side effects, insufficient dose or duration of treatment, poor adherence, or true treatment resistance would hinder optimal outcomes14. Besides, CBT has been shown effective for managing depression and anxiety with sustainable improvements. However, there are barriers to accessing treatment at the service level, such as a lack of resources, inadequate staff training, limited availability of age-specific treatments, difficulties in liaising with families, and perceived stigma15.
Given that no single treatment would effectively control anxiety disorders and other mental illnesses without any limitation, newer treatment options are needed to counter the disorders, either as monotherapies or combined with existing treatment.
Because of the unmet needs highlighted, safe and effective therapies for mental disorders with improved accessibility would help overcome the barriers to treatments for patients with anxiety disorders. Digital therapeutics (DTx), by definition, provides evidence-based therapeutic interventions by means of qualified software programs to prevent, manage, or treat medical conditions. They can be used as a monotherapy or in combination with other therapies, including medications or devices to improve outcomes16. In this regard, DTx would be a potential treatment option for managing anxiety disorders.
Although both can be involved in the management of diseases, it is essential not to confuse DTx with digital medicine, which typically optimises care by collecting health data and providing personalised information to either healthcare providers or consumers for guiding treatment decisions. Examples of digital medicine include digital diagnostics, digital biomarkers, and remote patient monitoring devices, whereas DTx, based on software programs, functions as medical device and is applied to the treatment of one or more medical purposes without hardware. Hence, DTx can be considered “software as a medical device” (SaMD)17. DTx frequently uses consumer mobile devices, such as smartphones and tablets, as mobile medical apps. DTx is regulatory-approved, prescribed therapeutic interventions to treat medical conditions18, though it does not require FDA-regulated hardware16.
Although DTx is relatively new in the clinical field, many clinical trials are undergoing in a broad range of physical and behavioural conditions such as diabetes, anxiety disorder, depression, insomnia, attention-deficit/hyperactivity disorder (ADHD), and substance use disorder17. Remarkably, a considerable number of DTx applications are emerging to treat mental health disorders.
Increasing awareness of one’s levels of anxiety and suggesting personalised health behaviours may relieve anxiety and improve mental well-being in people susceptible to anxiety disorders. In a randomised controlled trial (RCT) by Ponzo et al (2020), a mobile app (BioBase) was developed to enhance one’s mental well-being. The BioBase app comprised psychoeducational content on mental health and well-being, mood tracking, CBT and in-the-moment exercises, such as deep breathing and relaxation techniques. Alongside therapeutic content, data on physical activity, sleep quality, and heart rate are collected via a wrist-worn wearable device coupled with BioBase and made available to the individuals using the app to foster an increased awareness of the users’ current well-being19.
The RCT recruited 262 full-time undergraduate students in the UK, who were randomly assigned to receive a 4-week intervention with BioBase (n=130) or wait-list control (n=132). The psychoeducational content was delivered via 42 five-minute modules. Embedded in these modules are elements of CBT and self-compassion. Anxiety (represented by STAI-S-6 score) and perceived well-being (defined by WEMWBS score) of the participants were assessed with a self-reported questionnaire at four time points in the study period19.
The results demonstrated that the BioBase program significantly reduced anxiety and increased perceived well-being, with sustained effects at a 2-week follow-up (Figure 3A and 3B)19. The findings suggested that digital mental health interventions could constitute a novel approach to treating stress and anxiety. Further investigations combining digital therapeutics with existing therapeutic pathways are thus warranted.
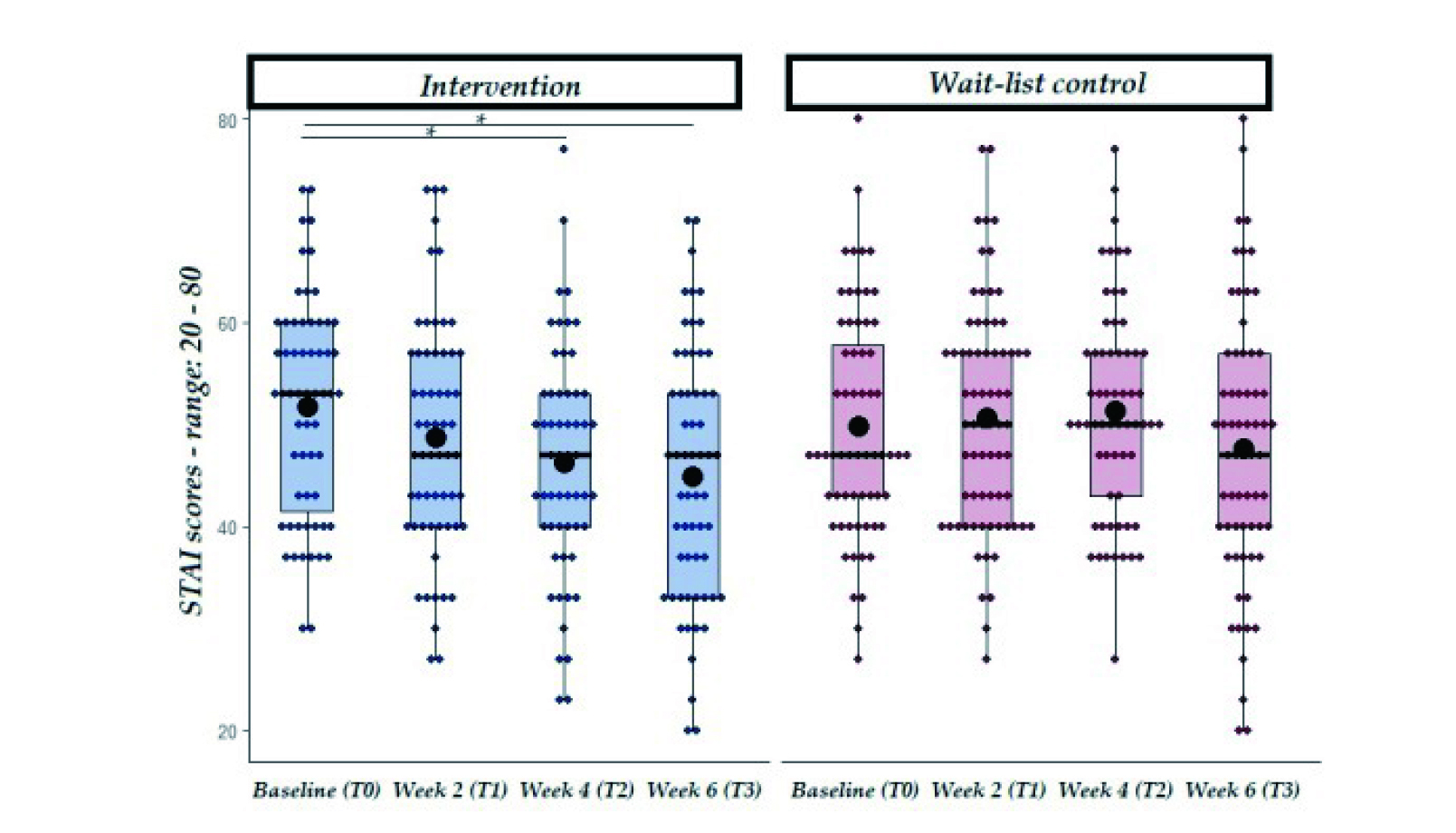
Figure 3A. STAI scores (anxiety) trends in intervention and wait-list control groups19, solid line: median; black dot: mean; *p<0.01
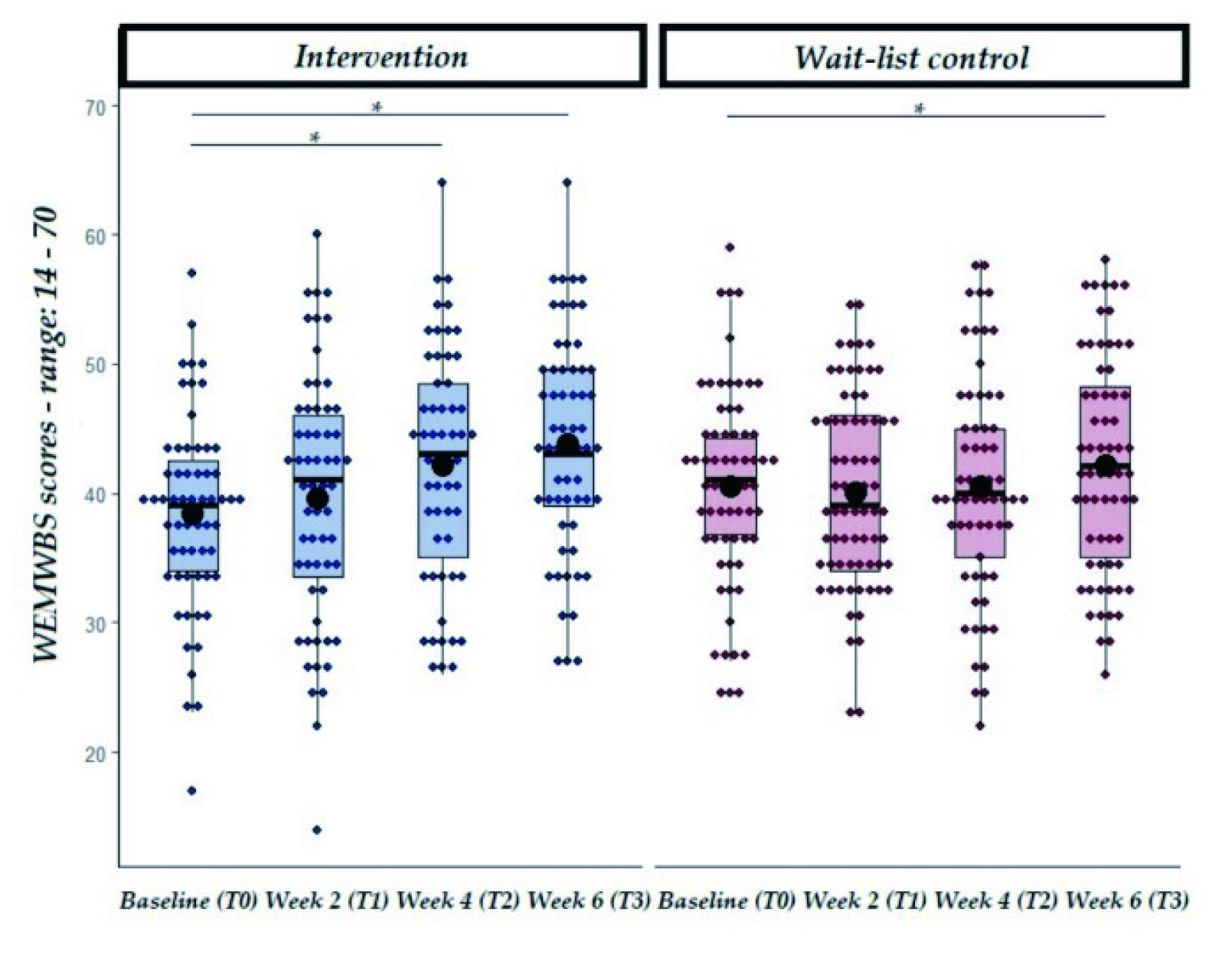
Figure 3B. WEMWBS scores (perceived well-being) trends in intervention and wait-list control groups19, solid line: median; black dot: mean; *p<0.01
Apart from foreign clinical data, a local study evaluating internet-based cognitive therapy for social anxiety disorder was conducted by Thew et al (2019). The study included training local therapists in delivering treatment with an internet-based therapeutic program (iCT-SAD), which was developed in the UK, and the subsequent treatment for six patients with social anxiety disorder20.
Most of the key learning of iCT-SAD treatment can be achieved by the patient’s self-study on the internet, facilitated by trained therapists. In the study, the therapists communicated with their patients using brief secure messages, telephone calls, and occasional webcam chats. The treatment lasted 14 weeks, followed by a 3-month booster period, during which the participants retained access to the program. The primary patient outcome measure was the self-report version of the Liebowitz Social Anxiety Scale (LSAS)20.
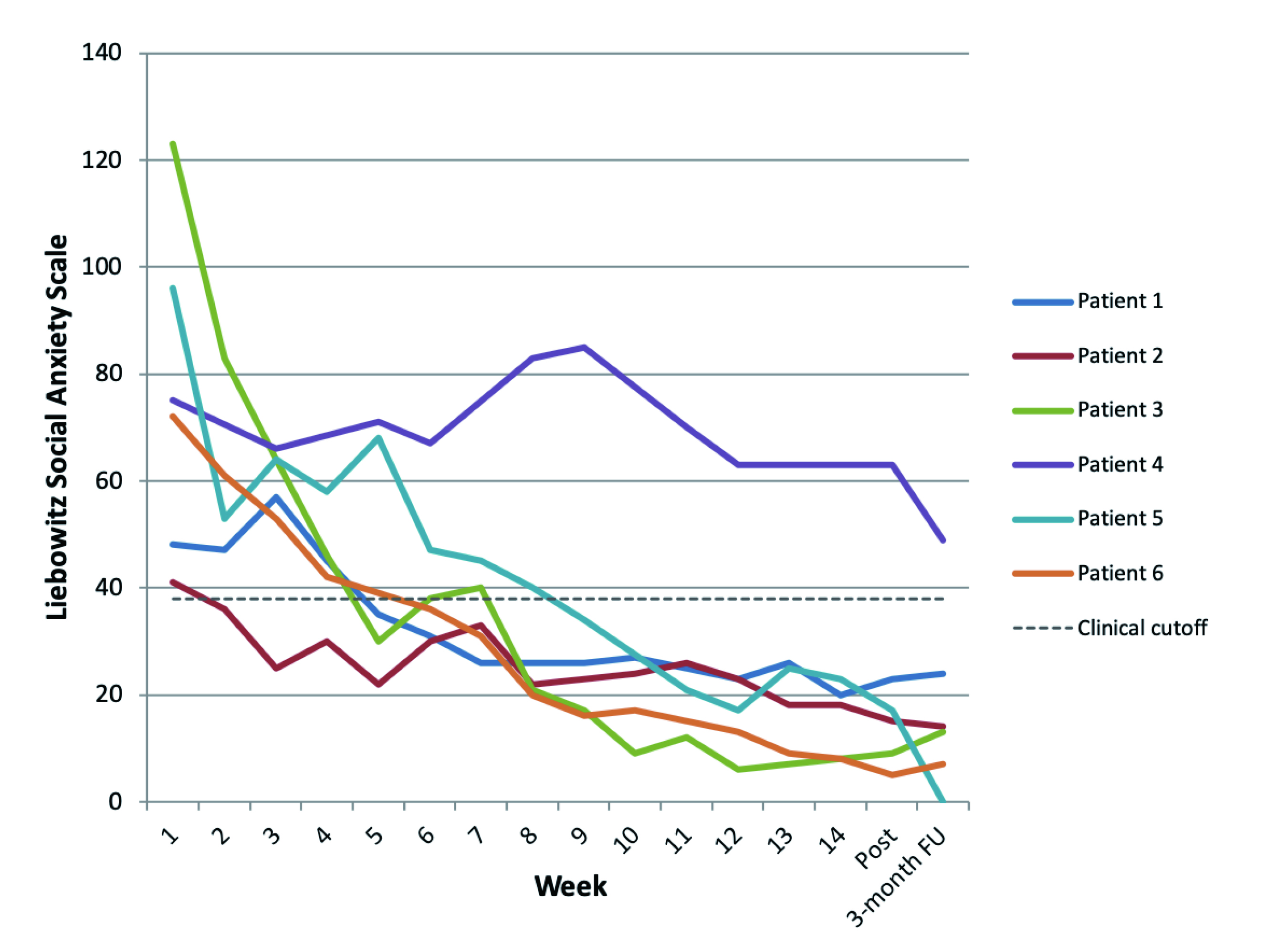
Figure 4. Self-reported LSAS scores across iCT-SAD treatment period20
The results reflected that the iCT-SAD program significantly improved LSAS scores in the patients. In addition, evidence suggested that the patient’s clinical outcomes were sustained at a 3-month follow-up (Figure 4). While the iCT-SAD program was developed in the UK, the patient and therapist feedback did not identify any significant cultural barriers to implementing the program in Hong Kong20. The results suggested that the internet intervention was promising in improving outcomes in patients with social anxiety disorder, whereas further evidence from RCT is desirable.
DTx represents a category of emerging treatment approaches which enriches the spectrum of therapeutic options in various medical conditions and is expected to significantly influence healthcare delivery globally. Remarkably, the therapeutics could potentially overcome some barriers for patients with mental disorders to access treatment, e.g. during a pandemic. Moreover, the therapeutic outcomes of DTx in combination with existing medications for anxiety disorders and other mental problems are worth further investigation. In conclusion, the continued rapid advancements in both the capabilities and availability of digital technologies would facilitate the development of novel, effective DTx products, which would in turn benefit patients with mental disorders.
References
1. Baxter et al. Psychol Med 2013; 43: 897–910. 2. Lam. Int J Psychiatry Clin Pract 2006; 10 Suppl 3: 18–24. 3. Yang et al. Epidemiol Psychiatr Sci 2021; 30. DOI:10.1017/S2045796021000275. 4. Department of Health. Let’s Talk About Anxiety Disorders. Non-Communicable Dis Watch 2019. 5. Craske et al. Depress Anxiety 2009; 26: 1066–85. 6. Craske et al. Anxiety disorders. Nat Rev Dis Prim 2017; 3. DOI:10.1038/NRDP.2017.24. 7. Zhao et al. Front Psychiatry 2021; 12: 715. 8. Hou et al. Soc Psychiatry Psychiatr Epidemiol 2021; 56: 1499–508. 9. Anxiety disorders - Diagnosis and treatment - Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/anxiety/diagnosis-treatment/drc-20350967 (accessed Nov 1, 2022). 10. Garakani et al. Front Psychiatry 2020; 11: 595584. 11. He et al. J Psychiatr Res 2019; 118: 21–30. 12. Bandelow et al. Dialogues Clin Neurosci 2017; 19:93. 13. Lam et al. Soc Psychiatry Psychiatr Epidemiol 2015; 50: 1379–88. 14. Farach et al. J Anxiety Disord 2012; 26: 833. 15. Wickersham et al. J Med Internet Res 2022; 24. DOI:10.2196/29842. 16. Hong et al. Comput Methods Programs Biomed 2021; 209. DOI:10.1016/J.CMPB.2021.106319. 17. Nwosu et al. Front psychiatry 2022; 13. DOI:10.3389/FPSYT.2022.900615. 18. Sverdlov et al. Clin Pharmacol Ther 2018; 104: 72–80. 19. Ponzo et al. JMIR mHealth uHealth 2020; 8. DOI:10.2196/17767. 20. Thew et al. JMIR Form Res 2019;3(2)e13446 https//formative.jmir.org/2019/2/e13446 2019; 3: e13446.





