
Service Director (Quality & Safety)
Hong Kong East Cluster
Hospital Authority

Adjunct Professor
The Jockey Club School of Public Health & Primary Care
The Chinese University of Hong Kong

Chief Manager
Patient Safety and Risk Management Department,
Quality & Safety Division
Hospital Authority
Patient safety and quality of care are the fundamental components of optimal healthcare. In particular, patient safety is paramount because any medical mishap may lead to life-threatening outcomes. In this regard, learning from past sentinel events, improving the clinical operation procedures, and promoting the safety culture are essential to building a safer healthcare system. During the International Forum on Quality and Safety in Healthcare Hong Kong 2024, organised between 26th-28th August 2024, Prof. Lui Siu Fai, Dr. Sara Ho, and Dr. Raymond Cheung jointly gave a speech titled “Sentinel Events of the Hospital Authority, Hong Kong - 17 years on, what have we learnt?”, which discussed the measures implemented by the Hospital Authority (HA) to support patient safety.
The Lesson from a Tragedy
A sentinel event is an unexpected occurrence involving death, serious physical, psychological injury or the risk thereof. Common sentinel events reported in clinical settings in literatures include unintended retention of a foreign object after invasive procedures, suicide or abduction of a patient receiving care, invasive procedure on the wrong patient, wrong site, haemolytic transfusion reaction, etc1.
Prof. Lui presented the sentinel event of an unintentional intrathecal (IT) administration of vincristine, which was intended for intravenous (IV) administration, to a 21-year-old female patient with acute lymphoblastic leukaemia (ALL) in the ambulatory care unit of a local public hospital in 2007. Upon achieving complete remission with induction chemotherapy, the patient proceeded with maintenance treatment according to the UK ALL XII protocol, which included IV vincristine and IT cytarabine2.
Being prescribed together on a prescription sheet and dispensed together to the ambulatory care unit, the medications were then put together on a trolley prepared for lumbar puncture (LP) and IT chemotherapy administration. Unfortunately, the doctor and the nurse were unaware that the vincristine dispensed in a pre-filled syringe was intended for IV injection. After that, the patient became ill and eventually succumbed to death from the error, which was confirmed 3 days after drug administration2.
“The patient fought bravely against leukaemia and was winning. But we (the hospital) made an error, and she could not survive,” Prof. Lui expressed. He stressed that the patient’s tragic death should not be in vain. Indeed, since the medical mishap back in 2007, the HA has implemented key systemic changes to reduce the risk of sentinel events.
Reported Sentinel Events in HA
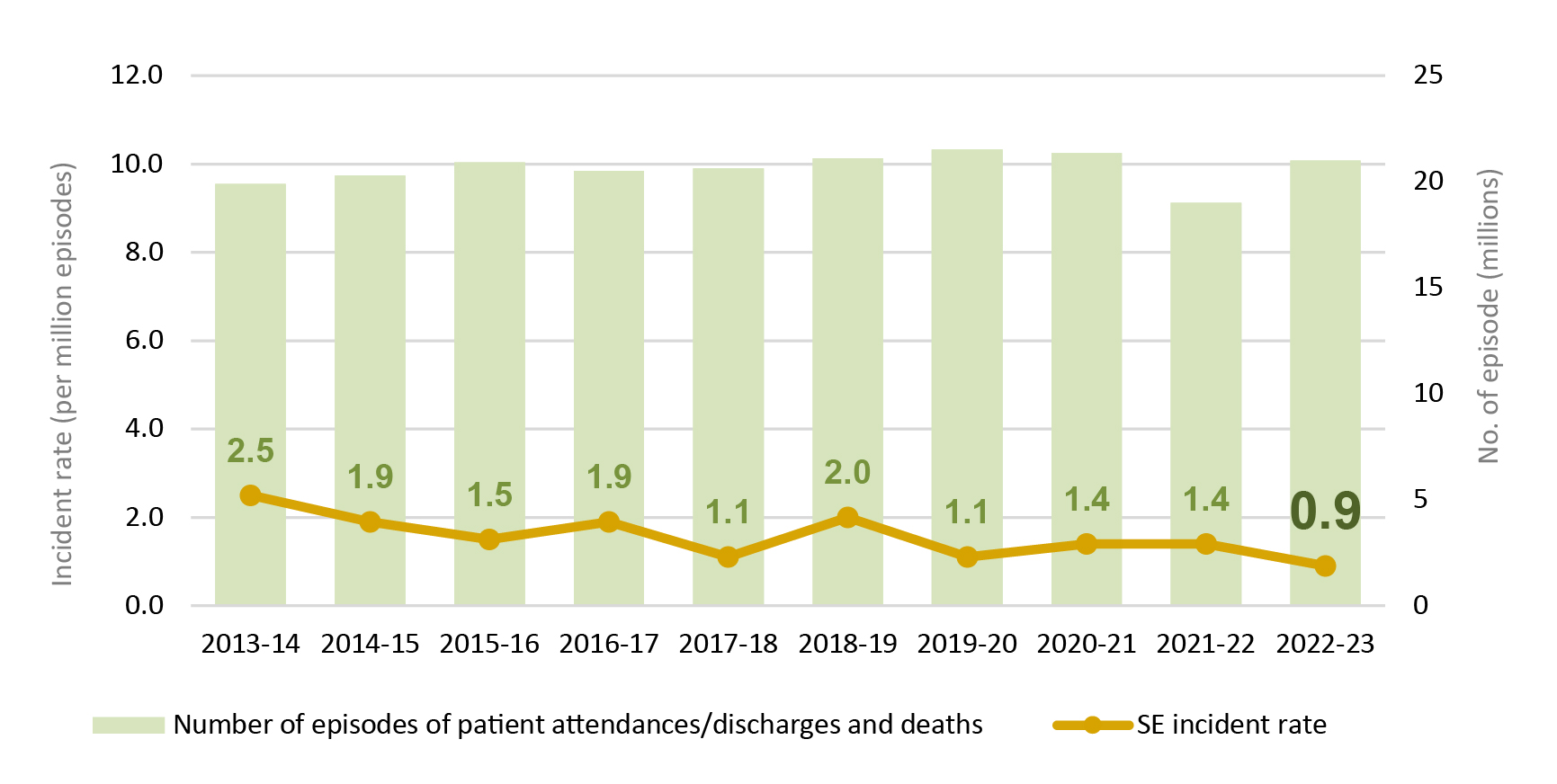
As per the statistics published by HA, a mildly decreasing trend in sentinel event incidence rate was observed in 2013-23, whereas the incidence rate in 2022-23 was 0.9 per million episodes (Figure 1). Dr. Ho further presented that the categories of retained instruments/material and in-patient suicide ranked as the top 2 most frequently reported sentinel events (Figure 2). Remarkably, 84% of sentinel events were reported in acute general hospitals with 24-hour accident and emergency (A&E) services in 2022-233.
Systemic Changes in HA – The Effort to Support Patient Safety
Dr. Ho stated that the most effective way to address the risk of sentinel events is to identify the underlying system-level issues. For instance, to increase staff awareness of sentinel events and maintain the confidence of public and regulatory bodies, HA introduced the Sentinel Event Policy to standardise the practice and procedures for handling sentinel events in all public hospitals, thereby strengthening the reporting, management and monitoring of sentinel events in public hospitals in 2007. The policy was revised to become the Sentinel and Serious Untoward Event (SE & SUE) Policy in 20104.
Essentially, the Head Office of HA consolidated its experience handling clinical incidents to ensure consistent interpretation and management of sentinel events by updating the SE & SUE Policy and issuing the Clinical Incident Management Manual (CIMM) in 20155. Dr. Ho highlighted that the CIMM provides guidance on reporting, investigating, analysing, and monitoring clinical incidents, whereas the CIMM is reviewed and updated regularly, and the latest review was commenced in 2023.
Besides, introducing new technologies is crucial for improving the operation procedures. For instance, Dr. Ho noted that the unique patient identification (UPI) device was applied in HA hospitals as an adjunct to the human checking process to ensure correct patient identification in blood transfusion.
Apart from retained instruments/material and in-patient suicide, Dr. Ho addressed that medication errors have made up a significant proportion of SUE cases (Figure 2)3. Accordingly, the in-patient medication order entry (IPMOE) system was first introduced in 2013 and has subsequently been expanded to cover all HA hospitals. Dr. Ho outlined that the IPMOE system is a computerised closed-loop control system covering the entire medication management process for HA in-patients.
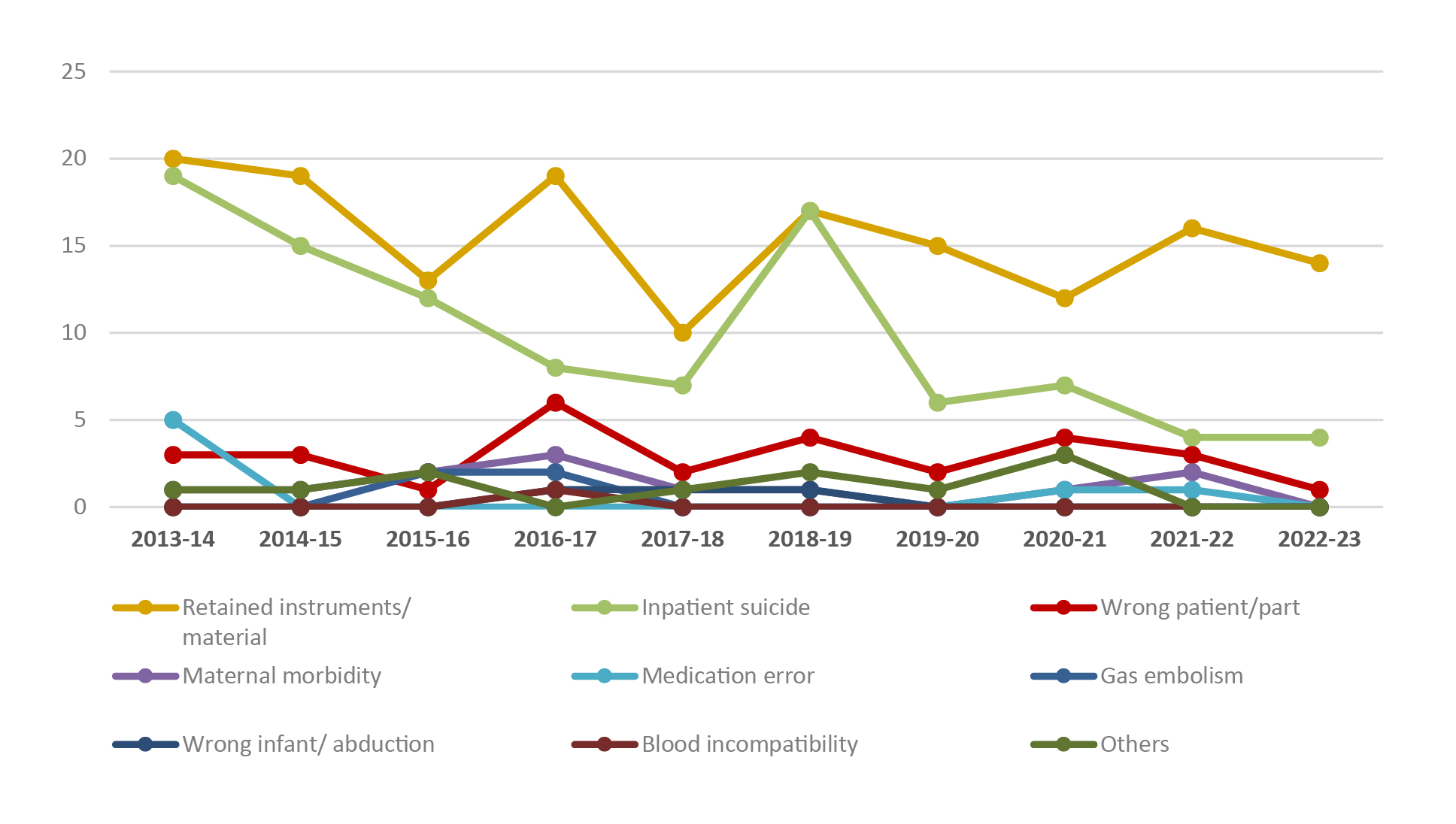
Figure 2. Number of sentinel events by category3
Notably, the IPMOE system has been enhanced based on the feedback from frontline staff. Medication decision support, which guides appropriate prescriptions by generating alert messages based on patients’ profiles, is one of the enhancements made to improve patient safety. Moreover, the enhanced operation system enables clinicians to proactively monitor high-risk patients when prescribing treatments.
Reviewing and Re-engineering for Reducing Future Sentinel Events
Given the path forward in reducing sentinel events, Dr. Cheung outlined that we need to re-visit the current practice, re-think the strategies, re-focus on the goals, and re-connect all people in the patient safety journey. He outlined that the HA reviewed its incident management framework and policy. In particular, the panel recommended inviting human factors and root cause analysis (RCA) experts and dedicated teams to conduct RCA. Also, strengthening the RCA training and using aggregate RCA format instead of performing for each case individually are recommended for selected incident categories.
Essentially, Dr. Cheung mentioned that, in cases of an incident, it is important for the staff members to recognise the issue and react immediately to control the risk. This concerns the development of a safety culture among all staff, and other stakeholders. Dr. Cheung opined that the centre of the patient safety culture is a just culture within the organisation, which emphasises management will support and reward reporting errors, whereas discipline occurs based on risk-taking. “Without this (just culture), the frontline staff might not be willing to report errors,” he commented. In addition, creating an environment for reporting would facilitate staff to report errors. The reporting platform should be simple and readily accessible.
While Dr. Ho highlighted the importance of system-based strategies in reducing sentinel events, Dr. Cheung added that subsequent implementation is crucial for bringing the strategies into reality. The implementation involves the management of changes, staff engagement and motivation. The re-engineering of workflow targeted the pain points of patients, carers, and staff. Collecting feedback, learning, and stakeholder engagement are essential during the re-engineering process. For instance, Dr. Cheung quoted the use of Global Trade Item Number (GTIN) on product packaging to accurately identify medications and reduce dispensing errors throughout the process.
Interestingly, Dr. Cheung introduced the idea that artificial intelligence (AI) and language models can be applied in various ways of incident investigation, such as data structuring, automated analysis, and summaries.
Conclusion
The clinical environment is complicated and dynamic so that clinicians are highly stressed, regardless of roles and disciplines. Sentinel events are unlikely to be eliminated, but measures have to be implemented to reduce their occurrence. In the past 17 years, the HA has learnt from past incidents and has analysed for interventions, such as the key systemic changes, to ensure patient safety.
In conclusion, Dr. Ho stressed that collaboration among clinical professionals, information technology teams, and policymakers is essential in optimising clinical operations. Regarding future development, Dr. Cheung looked forward to further improvement in the reporting system enhancing the 2-way communication between management and frontline colleagues. With the optimised reporting system and workflow refinement in HA, improved patient safety and reduced occurrence of sentinel events is foreseeable.
References
1. Zaboli et al. Int J Health Care Qual Assur 2018; 31: 575–86.
2. Hospital Authority. Report on a Medication Incident of Intrathecal Administration of Vincristine in Prince of Wales Hospital. 2007.
3. Hospital Authority. Annual Report on Sentinel & Serious Untoward Events. 2023.
4. Legislative Council. Mechanism for handling medical incidents in public and private hospitals . 2017.
5. Hospital Authority. Annual Report on Sentinel & Serious Untoward Events. 2016.





